You’ve probably had at least one ear infection in your life.
In fact, a 2006 study on ear infections found that almost 9 million children and teens in the United States contracted an ear infection that year.
Ear infections are more common in children than adults and are among the main reasons families visit a healthcare professional. Approximately 75% of children will contract at least one ear infection before the age of three years old.
Children are more prone to ear infections than adults because their horizontal eustachian tubes (the tube that connects our ears, nose, and throat) are shorter and narrower. This means it’s easier for viruses to find their way in and easier for the tube to get blocked.
Luckily ear infections in children are usually very minor. Adults can get ear infections too, and these are often minor but can sometimes lead to something more serious.
So what causes an ear infection, what are the symptoms, and how can you treat an ear infection? Read on to learn all about ear infections.
What is an Ear Infection?
An ear infection happens when a viral or bacterial infection occurs in the ear.
Ear infections, called otitis media in the medical community, can cause pain, inflammation, and fluid buildup. These infections are often painful because the inflammation and fluid buildup causes pressure on the eardrum.
Ear infections are categorized by the three parts of the ear:
- Outer ear infection
- Middle ear infection
- Inner ear infection
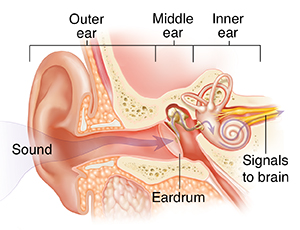
Source: https://www.saintlukeskc.org/health-library/middle-ear
These three types of ear infections have different causes and symptoms.
Outer Ear Infection
The outer ear extends from your eardrum to the outside of your head. In adults, the symptoms are simple. They usually experience ear pain and pressure, fluid in the ear, and reduced hearing.
Other outer ear infection symptoms include:
- Itchiness around ear
- Pain and tenderness in the ear
- Red and swollen appearance
- Fussiness in young infants
Outer ear infections are usually very minor and often resolve naturally, but occasionally they need to be treated with antibiotics.
Middle Ear Infection
The middle ear is the area right behind your eardrum. Middle ear infections are the most common and often happen when fluid gets trapped behind the eardrum. This causes the eardrum to bulge and infection to occur.
Symptoms of a middle ear infection include:
- Pain or discomfort
- A feeling of fullness in the ear
- Fluid drainage from the affected ear
- Fever
- Difficulty hearing
Most people will experience a middle ear infection at least once in their life. These infections are usually nothing to worry about, but it’s always a good idea to visit a medical professional to determine if antibiotics are needed.
Inner Ear Infection
The inner ear is behind our eardrum, located between the middle ear and the internal auditory canal. An inner ear infection is usually not a true infection. Often, symptoms presenting as an inner ear infection are actually a case of inflammation in the area of our ears responsible for balance and hearing.
Less commonly, an inner ear infection is a real infection. Symptoms of an inner ear infection include:
- Dizziness
- Problems with balance
- Nausea
- Hearing loss
- Fever
- Vomiting and diarrhea (more common in infants)
Inner ear infections are the least common, and they can become serious. Inner ear infections should always be examined by a medical professional.
What Causes an Ear Infection
Ear infections typically begin with a cold, flu, or allergic reaction, which increases mucus in the sinuses. The sinuses are connected to our ears and throat by the eustachian tube. When you have nasal congestion from a cold that begins to clear, your eustachian tubes allow the mucus to drain.
Eustachian tubes are small in size and run from each ear directly to the back of the throat. When the eustachian tubes get blocked or swollen with mucus, an ear infection occurs. This can also inflame the nasal passages and throat.
While colds, flu, and allergies are the most common cause of eustachian tube blockages, they can also be caused by infected or swollen adenoids and air pressure changes.
High Risks for Ear Infections
As discussed earlier, infants and young children have short and narrow eustachian tubes, which puts them at higher risk for ear infections.
Some adults have very narrow eustachian tubes or tubes that have not developed a slope. These adults are also at a higher risk for eustachian tube blockages.
If you experience seasonal allergies, you may also develop ear infections from nasal congestion and sinus blockages. Lifestyle habits like smoking can increase the likelihood of eustachian tube blockages and increase the risk of ear infections.
Ear Infection Diagnosis
Although ear infections are usually minor, it’s always a good idea to seek a medical professional’s advice. After asking questions about your symptoms, a medical professional will examine your ear with an instrument called an otoscope.
Otoscopes have a magnifying lens and light, which helps take a detailed look at your ear and your eardrum. Your medical professional may choose to use a pneumatic otoscope that emits a puff of air in the ear. This puff of air causes the eardrum to react and helps your medical professional make their diagnosis.
If the eardrum moves easily, it means you don’t have a middle ear infection, at least not a serious one. When the eardrum barely moves, it shows that there is fluid pressing against it from the inside.
Your medical professional can also do a simple hearing test to identify an ear infection, especially if one of the symptoms is hearing loss.
In more severe cases of ear infections, or if the symptoms are unusual, your medical professional may use a medical test called tympanometry. Tympanometry is another test done to diagnose and evaluate ear infections. These tests can discover:
- Redness, air bubbles, or pus-like drainage in the middle ear
- Damage in the eardrum
- Swollen or collapsed eardrum
In severe cases, your medical professional may take fluid samples from your ear to examine if the fluids contain antibiotic-resistant bacteria. However, this is very rare.
Treating an Ear Infection
In minor cases of ear infections, the body’s immune system can fight the infectious bacteria without the help of antibiotics. In some cases where the infection has progressed, or if you are experiencing a lot of pain and discomfort, your medical professional will prescribe antibiotics such as amoxicillin.
If you are prescribed antibiotics, you must complete the entire course of antibiotics, even if you start feeling better before finishing with the allotted doses.
In rare and severe cases of ear infections where antibiotics aren’t effective, your medical professional may recommend surgery. If you have many ear infections over a short period, your medical professional may recommend placing a tube in your affected ear to allow fluid to drain out more easily.
What Happens if an Ear Infection is Left Untreated?
While many ear infections resolve on their own, some cases do not, and it can be dangerous to leave these untreated. If your ear infection symptoms don’t improve or get worse, you should immediately schedule an appointment with a medical professional.
When severe ear infections are left untreated, they can cause hearing loss and ruptured eardrums. In extreme cases, an ear infection can lead to meningitis or neurological issues if left untreated.
If you or a loved one has an ear infection, there’s no reason to stress. If you seek medical help, ear infections are only minor discomforts that usually go away quickly.
Think You Have an Ear Infection?
If you’re concerned you have an ear infection, book an appointment with a medical professional at CityHealth Urgent Care today. We have locations in San Leandro and Oakland ready to help you get better.
If you think you have an ear infection but are experiencing only minor discomfort, you may be able to book a virtual visit to discuss your symptoms with a medical professional. A virtual appointment can help determine if you need an in-person appointment based on your symptoms.